Rising Measles Cases Spark Urgent Vaccine Questions | Image Source: abc7.com
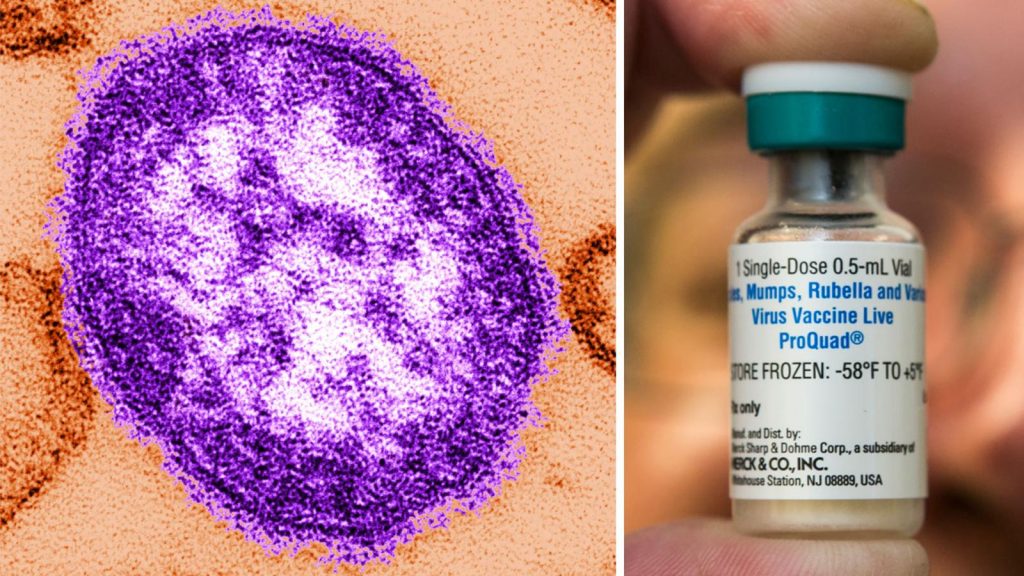
WASHINGTON, D.C., March 31, 2025 – As the United States clings to an increasing number of measles cases, a new wave of public health issues is emerging. With more than 483 confirmed cases reported across the country at the end of March – many of them in Texas, New Mexico and Oklahoma – Americans ask to understand: Do I still have immunity? Should I receive another dose of measles vaccine?
According to several sources of public health, including the Centres for Disease Control and Prevention (CDC), most adults do not require an additional dose. However, this safety is accompanied by some important exceptions. According to information from Gizmodo, The Conversation, ABC News and NEPM, MMR vaccine (medial, mumps and rubella) remains the gold standard for protection. However, recent epidemics are prompting experts to clarify exactly who should consider additional fire, and why this is more important than ever.
Why is measles coming back?
Once declared eliminated in the United States in 2000, measles returned, exploiting the vulnerabilities of immunization coverage. According to the CDC, more than 90% of recent cases have occurred in unvaccinated individuals, particularly in communities that avoid vaccines because of their personal beliefs or face barriers to access to health. Current outbreaks have reached over 500 confirmed cases, and epidemiologists believe that the actual number can be higher because it is not reported.
Measles is one of the most contagious viruses on the planet. It spreads through the air, an infected person can infect up to 18 people in an unvaccinated population. Symptoms – fever, cough, rash, and in severe cases, inflammation of the brain (encephalitis) – make less a benign childhood disease. During the pre-vaccinal period, the United States saw tens of thousands of measles-related hospitalizations each year.
“The virus does not concern itself with borders or beliefs,” said Dr. Walter Orenstein of Emory University, a former CDC official. “Aflora when you find unvaccinated individuals. That is why Community immunity is so critical that it concerns not only personal protection, but also the protection of those who cannot be vaccinated for medical reasons.”
Who should consider another dose of measles vaccine?
Not everyone needs another dose, but there are clearly defined exceptions. Adults born before 1957 are usually presumed to be immune, as they probably contracted measles in childhood prior to the vaccine. According to Dr Paul Offit of the Philadelphia Children’s Hospital, these people are not advised to be vaccinated unless specific medical concerns arise.
However, adults born between 1963 and 1967 occupy a grey area. Over the years, an inactivated measles vaccine has now been administered. Unfortunately, it provided short-term immunity and in some cases resulted in atypical and more serious reactions to infection. If you have been vaccinated within this time frame and are unsure of the type of vaccine you have received, the CDC recommends at least one dose of the current attenuated live MRM vaccine.
“This is not an excessive reaction,” said Dr. Gregory Poland of the Atria Research Institute. “It’s about being informed. If you fall into this early vaccination history window and cannot check the type of vaccine, the safest option is to revaccinate
Is two doses enough for life?
For most people, yes. The two-dose MMR diet, introduced universally in 1989, provides approximately 97% of measles efficacy. Even a single dose offers about 93% protection. Immunization immunity is durable and generally does not disappear significantly over time. Studies estimate a negligible decrease in efficacy between 0.04% and 0.22% per year. This means that it will take decades to lose only 1% of protection.
“The idea of a booster is a little misleading,” said Dr. Offit. “The second dose was implemented not because immunity was waning, but because many children forgot the first dose. The second shot only claims that they did not fall into the cracks. “
However, some high-risk groups are advised to obtain a second dose if they have received only one dose. These include health workers, international travellers, university students and people living in outbreak areas. For example, Amber Black, a resident of Massachusetts travelling to Texas, chose to be vaccinated after a blood test showed no detectable immunity. He felt responsible, he said. “I can be fine, but it’s about protecting those who are not.”
Can you check your immunity?
Yes, but continue with caution. Antibodies tests, also called titre tests, may indicate if you still have measurable antibodies against measles. But here is the capture: antibodies are only part of the memory of the immune system. It is not because the antibodies are weak that you are not protected. Your body can still accommodate memory B cells and action-ready T cells.
“The evidence against the body can be misleading,” said Dr. Daniel Pastula of the University of Colorado. “A low outcome does not always mean vulnerability. It depends more than the test can show.”
For most people, especially those who do not have high-risk work or travel abroad, repudiation or re-vaccination is not necessary unless they are not sure of their past. Immunization records can be found in government immunization records, past medical records or even school records. In cases where records are missing and there is a high risk, it is perfectly safe to get another dose of RRO vaccine, even if it is already protected.
Can the vaccine cause measles?
That’s not true. It’s a myth. The MMR vaccine uses a live but severely weakened virus that is unable to cause a true measles. It may cause minor symptoms in some people, such as low-grade fever, rash or joint pain, but these side effects are short-lived and much milder than a real infection. CDC and Texas health officials confirmed that the current outbreak was caused by a wild type virus, particularly genotype D8, and not by the vaccine strain, genotype A.
“This is not the failure of the vaccine,” said Dr. Poland. “This is the failure to vaccinate. Science is solid. The protection is strong. What we see now is the result of doubt, not technology
What about young children and extra doses?
Children usually receive their first dose of RRO between 12 and 15 months, followed by a second dose between 4 and 6 years. However, in areas such as Texas, public health officials have allowed a first and third dose for babies between 6 and 11 months. This is not a replacement, but an additional precautionary injection.
Dr. Poland said this early dose is not a standard protocol. “It’s for babies in high-risk areas or those travelling in these areas. Maternal antibodies may affect the efficacy of the vaccine if administered too early, so that the initial dose is not counted in the two-dose routine series. »
In other words, babies receiving an early dose due to the risk of exposure will still need the two usual injections later in life to ensure long-term immunity.
What if you’re not sure?
If you are wondering when or if you have MMR vaccine, the first step is to check your records. By not doing so, and especially if you enter a high risk scenario - such as an international trip or living near an epidemic – it is prudent to consult your doctor. And if the files are missing or unclear, getting another MMR shot is a safe and effective way to close the gap.
No need for panic, but there are reasons to act. Your vaccine is not just about you. It is a shield for everyone around you, especially for babies too young for vaccines, patients with medium-treatment cancer and the older neighbour with a compromised immune system.
The virus thrives in uncertainty and complacency. But with clear knowledge and accessible vaccines, Americans can cut off the short transmission chain. As the doctor said. Orenstein, “High levels of vaccination not only protect vaccinees – they protect everyone. That’s how we stop the buds. ”