Ketamine’s Double-Edged Rise in Mental Health Care | Image Source: www.talkingdrugs.org
BILLETS, Montana, 25 March 2025 – An increased interest in the role of ketamine in mental health therapy emerged after a tragic incident in Wyoming, where a mother, who allegedly received ketamine for depression, killed her four children and herself. Toxicological reports have indicated significant levels of ketamine in your system, starting an intense debate about the dual identity of the substance, a powerful medical tool and a potentially dangerous drug when used inappropriately. As mental health professionals and researchers struggle to define their limits, the increasing use of ketamine in psychiatry creates both hope and concern.
What is Ketamine, and why is it used for depression?
Originally developed in the 1960s as an alternative anesthesia, ketamine has long been used safely in controlled medical environments for surgery and pain relief. According to Dr.Erin Amato, a psychiatrist at the Montana Centre for Psychiatry and Brain Health, began to be marked in mental health treatment in 2016, especially for treatment-resistant depression (RTD) cases in which conventional drugs such as SSRIs do not provide relief. “It’s a treatment for depression and even PTSD in outpatient clinics,” said Dr. J’aime MTN News, noting that ketamine is generally considered after several other options have been exhausted.
Ketamine is administered by intravenous infusion or nasal spray. While the FDA only approved the nasal spray version, Dr. Amato reports remarkable results: ”The inequality of 80% of people who report a 50% improvement in their symptoms of depression,” he said. Patients often describe their post-treatment relief as a distant cry of the week-long wait period associated with traditional antidepressants.
What are the risks of ketamine treatment?
Despite its potential, ketamine is not without inconvenience. According to Dr. Amato, treatment should be carefully monitored. “It is really important that it be administered in a medical setting,” he said. Side effects may include an increase in blood pressure, nausea, dizziness and a sense of dissociation from reality – the so-called “dissociative” state that has made ketamine popular in night scenes.
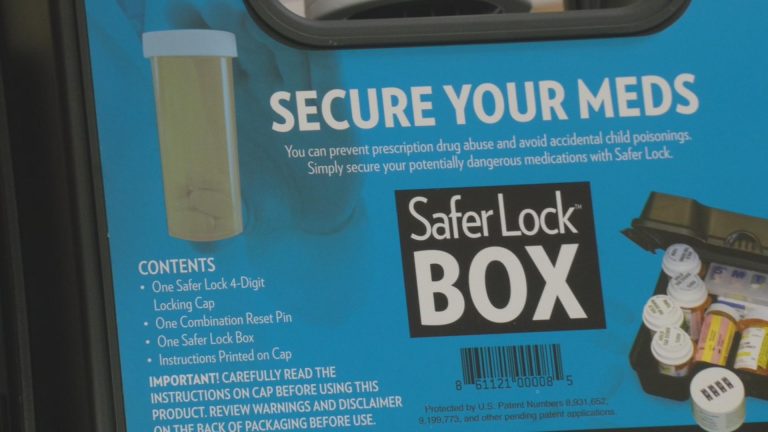
There is an additional complication: online startups now offer ketamine therapies at home, raising red flags among doctors. This is where I am very nervous, Amato added, stressing that ketamine is a controlled substance with the potential for abuse or distraction. When it is misused, especially in unsupervised environments, its effects may fall into dangerous territory.
How do researchers expand the range of ketamine?
In Christchurch, New Zealand, an innovative essay conducted by associate professor Ben Beaglehole at the University of Otago combines oral ketamine with behavioural activation therapy (ART). The purpose of the trial is to fill a significant gap in the current treatment of ketamine – relapse. “Kétamine is probably the most exciting new treatment for a generation of depression,” said Beaglehole. However, many patients are reluctant shortly after stopping the drug, leaving a hole in the long-term care strategy.
BAT is designed to counter depression-induced inactivity, encouraging patients to return to their daily lives. The current study involves 60 patients receiving oral ketamine and/or BT for eight weeks, followed by a 12-week observation period. Preliminary results are promising but inconclusive, as only half of the target group of participants was recorded. The goal is not only to extend remission, but to understand whether behavioural support can provide lasting mental health scaffolding after treatment has been completed.
How is oral ketamine compared to intravenous use?
Most previous studies focus on intravenous ketamine (IV), which tends to cause a rapid and intense dissociative effect. Otago judgment, however, uses oral ketamine, which is slower, softer, and can reduce the likelihood of negative psychological reactions. “Participants receive ketamine to swallow, which reduces the effect of a one-way ride,” said Beaglehole. This subtle but important change in delivery could redefine how and where ketamine is administered, making it more accessible without compromising safety.
However, Beaglehole warns that this journey is not without emotional turbulence. ”The study can be a bit of a Russian mountain,” he said, recognizing that participants who respond well can fight after the treatment phase, especially in the absence of continuous access.
Is ketamine effective for other mental disorders?
Yes, and their applications grow fast. According to TalkingDrugs and Pharmacy Today, ketamine trials are now under study for Obsessive-Compulsive Disorder (OCD), Post-Traumatic Stress Disorder (PTSD), and even eating disorders such as nerve anorexia. The EDEN project (Ketamine for depression with anorexia Nervosa), for example, administers oral ketamine and psychoeducation to relieve symptoms of depression in patients with persistent anorexia, a population for which treatment options are significantly limited.
Dr. Johanna Keeler, EDEN Test Director, notes the delicate balance in prescribing ketamine to vulnerable populations. “This is particularly important in psychiatric populations where abuse may pose a particular risk,” he explained, noting that while abuse is more often associated with bulimia, all participants in the study are carefully analyzed and monitored. This level of caution, he insists, is necessary to distinguish therapeutic use from recreational violence, a critical challenge for perception and policy.
Can ketamine help treat addiction?
Intriguingly, yes. MORE-KARE – an acronym for Ketamine Multi-Central Research for Alcohol Recaid Reduction – investigates whether ketamine combined with psychotherapy can reduce relapse rates in people with alcohol use disorders. The therapy works at several levels: physiologically, due to the damping of anxiety; and psychologically, improve engagement during therapeutic sessions. The researchers argue that the dissociative effects of ketamine can create a mental “restart” allowing patients to see their behaviour through a new lens.
This study follows a similar therapeutic model known as ketamine-assisted psychotherapy (KAP), where patients receive a low dose of ketamine in a guided environment. By temporarily interrupting harmful loops of thought, KAP aims to open emotional and cognitive doors that traditional therapy often struggles to germinate. For addiction specialists, this is a hope – though cautiously optimistic – in addition to the recovery toolkit.
Are there safer alternatives to ketamine on the horizon?
Yeah, and they’re already in clinical trials. The National Health Institutes recently conducted a Phase 1 study on a metabolite of ketamine known as (2R, 6R) – Hydroxynorketamine (RR-HNK). Unlike ketamine, RR-HNK does not cause dissociation or sedation, making it a promising candidate for long-term safe use. The study included 74 participants and revealed no serious adverse reactions, with blood clearance within eight hours. If future studies confirm their effectiveness, RR-HNK may become a less controversial but also effective antidepressant.
Another medicine, L-655.708, also attracts attention. Previously explored to improve cognitive performance, it acts on GABA receptors – increasing glutamate levels in the brain similar to ketamine but without hallucinogenic side effects. These new compounds could one day offer the advantages of ketamine without its drawbacks, widening the pharmacological landscape of DRT.
What are the legal and social barriers to the use of ketamine?
Despite encouraging clinical data, the use of ketamine in psychiatry remains politically and socially marked. In January 2025, the United Kingdom National Office proposed to examine the legal status of ketamine, which could move from a class B subject to a class A subject. This measure, if adopted, could seriously impede access to medical research and treatment. Keeler expressed his concern, but he remained pragmatic: “It’s not necessarily a barrier,” he said, noting that other Class A substances such as psilocybine have been studied under special licence.
Public perception remains another major obstacle. Mediated deaths often spread the lines between medical use and abuse, casting shadows on legitimate research. According to Dr. Keeler, the real challenge is not to legitimize ketamine as a well-established anesthetic, but to promote its psychiatric use without stigma. “Better protection and surveillance measures can help increase confidence in their use,” he said.
How does ketamine work in the brain?
Unlike SSRIs that increase serotonin over time, ketamine acts through completely different neuronal mechanisms. It blocks NMDA receptors, improves glutamate release and triggers a cascade that increases neuroplicity - the brain’s ability to relive. It also increases brain-derived neurotrophic factor (BDNF) levels, promoting resilience and regeneration in brain areas such as prefrontal cortex. In short, ketamine not only raises mood, but it reshapes the architecture of thought.
These quick action benefits make ketamine attractive, especially for those caught in deep depressive episodes. However, its short duration means that repeated doses are often necessary, causing logistical and security problems. Other solutions such as RR-HNK could maintain these effects without requiring continuous infusions or addiction problems.
In the evolutionary landscape of psychiatric medicine, the rise of ketamine is as complicated as it is fascinating. As researchers continue to study their many dimensions – from depression and PTSD to anorexia and addiction – drug theatres between revolutionary tool and risky bet. Physicians, decision makers and patients will have to find this delicate balance with caution, compassion and openness.