The Hidden Crisis Behind Methadone’s Red Tape | Image Source: www.rstreet.org
WASHINGTON, D.C., April 2, 2025 – A powerful coalition of drug medicine advocates, policy experts and bipartite think tanks urges the Trump administration to reduce the administrative burdens that continue to alter access to methadone, a drug tested to prevent opioid-related deaths. In an open letter to management, the group asked the Department of Effectiveness of the United States Government to use its deregulation mandate to modernize access to methadone and its distribution, citing the potential of the drug to significantly reduce overdose deaths in the United States.
Although methadone has been the cornerstone of the treatment of opioid use disorder (ODD) since the 1960s, strict federal and state regulations have transformed it into a paradox: a drug that saves lives taken hostage by bureaucratic obstacles. Critics often like the current system to be punished rather than a path to recovery. Many patients have stabbed methadone with “liquid layers”, not because of the drug itself, but because of the way it is distributed, strictly controlled by highly regulated opioid treatment programs (POTs) that require daily visits, extensive communications and financial costs that many cannot bear. These policies, according to critics, are not only outmoded, they are deadly.
Why is methadone so limited compared to other medicines?
According to drug experts, methadone is an opioid per se, raising concerns about abuse and diversion. But unlike heroin or fentanyl, methadone is slow and lasting. Instead of rushing to euphoria, it provides a sense of normality, a desire for healing and avoids withdrawal symptoms. This makes it ideal to stabilize people in recovery. According to R Street Institute data, methadone treatment reduces the risk of overdose by 80% and significantly reduces rates of illicit drug use and criminal behaviour in patients.
However, the federal law requires methadone to be used only in specialized BTP clinics that meet their own strict standards. While this framework was initially intended to prevent abuse, critics now argue that it does more harm than good. OAPs are few and far from here, with over 80 percent of U.S. counties not even having clinics. For many, treatment involves time changes and frequent visits that interrupt work, school and parental responsibilities.
How does regulation make recovery more difficult, not easier?
Patients often have to go to the PCTs for up to six days a week to receive their drug under surveillance, a system that encourages not to depend on the drug but on the clinic. These barriers discourage many people from seeking or staying in treatment. As advocates say, even patients who are making long-term progress often face barriers to receiving home doses due to restrictive state or clinical policies despite recent federal flexibility.
Moreover, the experience of an OTP can demoralize. Patients are often subjected to scheduled counselling sessions that do not reflect individual needs, observed urine tests that feel invasive and zero tolerance rules for relapses, a swampy approach when addiction is recognized as a chronic relapse disease. “Imagine denying diabetic insulin because they had dessert,” said a drug addict at a recent symposium.
How much does methadone treatment cost?
Even if you manage to navigate in the glove of logistical obstacles, the financial burden remains considerable. Although methadone is relatively cheap as a drug, the associated costs, clinical fees, mandatory counselling, frequent testing, transportation and even child care can increase monthly costs from $300 to $500. The drug is often the most comprehensive payer, but the coverage is inconsistent, and many private insurers exclude PTO-based methadone from their plans. According to the R Street Institute, this leads to disparities in access, particularly for low-income patients, rural residents and people of colour.
Why has this system not changed, despite the overdose crisis?
Regulatory inertia and polarized political debates have hampered progress. Some policymakers advocate strict controls to prevent diversion, while others call for the total dismantling of medium-term plans, which have paralysed important reforms. Meanwhile, the overdose of opiates continues to take more than 165 lives a day in the United States. According to Stat News, 2024 has seen more than 60,000 such deaths, a decrease in previous years but still alarming.
Instead of choosing between overregulation and deregulated chaos, the experts propose an intermediate route: they allow doctors trained in drug addiction to prescribe methadone and allow pharmacies to distribute it. This approach, already used in countries such as Australia and the United Kingdom, could significantly expand access without sacrificing security. According to models cited by defenders, this change could reach 12 per cent of urban areas, 18 per cent of suburban areas and 16 per cent of rural areas currently serving the Office of the Prosecutor.
Can access be extended safely?
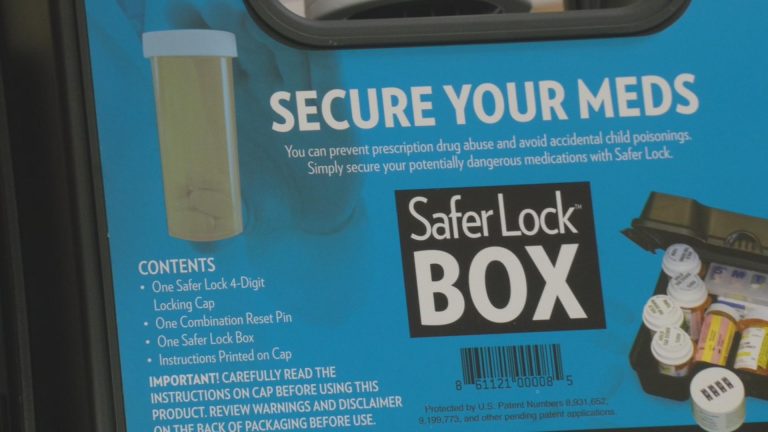
Yes, and there is a precedent. During the VOCID-19 pandemic, federal agencies temporarily released methadone restrictions to reduce in-person visits. Studies of these changes have not shown an increase in differences or negative results, which has led many experts to advocate ongoing reforms. In addition, new technologies such as telemedicine, digital adhesion tools and electronically blocked storage boxes offer innovative solutions to monitor patients remotely and ensure their safe use.
For patients who prefer the structure or for whom surveillance remains medically recommended, clinical and pharmaceutical programs may coexist. The dose of Pharmacy under professional supervision could be used as a means for those who are not ready for full privileges to return home but cannot engage in daily visits to the OTP. Such hybrid models would improve choice and reduce barriers by respecting the unique needs of each patient.
How does this fit the political objectives of the Trump administration?
The proposed changes resonate strongly with President Donald J. Trump’s February 19 Order in Council entitled “Ensuring Legal Governance and Implementing the President’s Government Regulatory Initiative”. This order focuses on reducing the federal regulatory burden, promoting competition and increasing the independence of suppliers and patients. Metadone reform, defenders’ argument, check all these boxes. It would eliminate unnecessary red tape, open up new contracts for the provision of treatment and allow health care providers to provide personalized care without interference from the old regulations.
According to the coalition letter, expanding access to methadone by pharmacies and qualified physicians does not eliminate the OTP model, but simply adds options. More importantly, it allows patients and providers to decide on the best treatment without being framed in a rigid and unique system. “We do not advocate chaos,” said one signatory. “We advocate election.”
What about methadone reform?
While federal agencies have shown signs of loosening the rules around methadone, lasting change requires state cooperation. Many states have laws that go beyond federal guidelines and effectively overcome federal, even progressive, changes. Advocates call on states to harmonize their policies with federal standards to remove barriers to access and improve care. Without such alignment, federal reforms will remain at best symbolic.
In the short term, some states may explore pilot programs, such as allowing primary care physicians certified in addictive medicine to prescribe methadone. Others may update their licensing criteria to encourage new clinics in underserved areas or experiment with drug dosing models. These progressive measures could pave the way for broader reform, demonstrating that security and access need not necessarily be mutually exclusive.
Ultimately, methadone reform is not just a matter of technical health policy, but a moral and humanitarian imperative. Every delay, every bureaucratic obstacle, every forced communication has a cost, often paid in human life. As the defence coalition stated in its letter, “the overdose crisis requires more than talking, it requires a transformation.” For now, the country is at a crossroads: continuing to cling to a broken system, or taking bold and evidence-based actions to save lives. The decision must be clear.